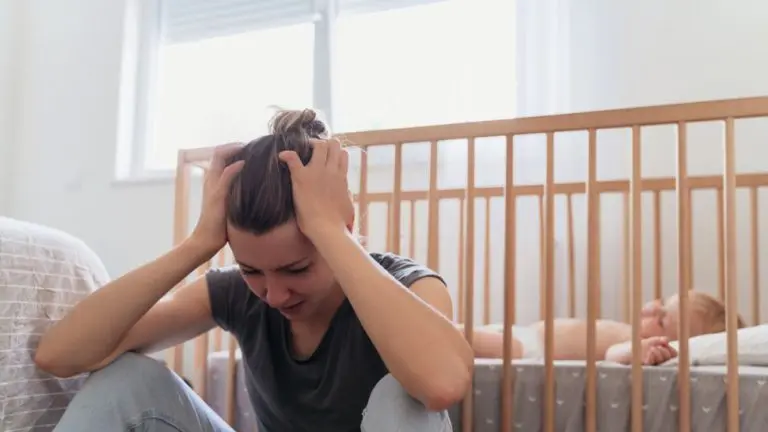
Childbirth and pregnancy are complex and exhausting processes for the mother’s body. During pregnancy, a woman goes through many hormonal, physical, emotional and psychological changes. Significant changes occur in her family and social life. After giving birth, the mother may experience a variety of emotions, ranging from joy and pleasure to sadness and bouts of crying. This emotional imbalance, called the “baby blues,” usually begins to subside within the first 2 weeks after birth.
It has been found that around one in seven women develop postpartum depression. While women who experience the baby blues recover quickly, postpartum depression is more prolonged and seriously affects their ability to return to everyday life. Postpartum depression has a negative impact on the health of the mother and her relationship with the baby .
Postpartum depression most often occurs within 6 weeks of giving birth. This condition occurs in about 6.5% to 20% of postpartum patients. The pathogenesis of postpartum depression is still not fully understood. Genetic factors, hormonal, psychological and social stressors are thought to play a key role.
The role of sex hormones in depressive behavior suggests a neuroendocrine genesis of postpartum depression. Changes in the levels of sex hormones hormones favor the dysregulation of emotional balance in predisposed women. It is known that the hypothalamus-pituitary-adrenal axis is involved in the pathogenetic processes of postpartum depression. This axis is important for the release of cortisol under stress , and if its function is impaired, then the natural response to stressful situations is also impaired. Hormones released in the function of the hypothalamic-pituitary-adrenal axis increase during pregnancy and remain elevated until 12 weeks postpartum.
Rapid changes in the levels of sex hormones, such as estradiol and progesterone, after childbirth can be a potential stressor in some patients, and these changes can lead to the onset of depressive symptoms . Oxytocin and prolactin also have an important role in the pathogenesis of postpartum depression. These hormones regulate the reflex for secretion and synthesis of breast milk. The inability to breastfeed and the onset of postpartum depression have been found to occur at the same time. Low levels of oxytocin are observed in patients with postpartum depression and those requiring early cessation of breastfeeding . During the third trimester of pregnancy, lower oxytocin levels are associated with an increased risk of depressive symptoms both during pregnancy and postpartum.
Sometimes the phase of postpartum depression in almost 30% of patients can last up to two years after childbirth , while in 50% of patients severe depression is observed throughout the time, in which the course of the condition can vary and stable moderate depression can be observed. severe stable depression or recurrent episodes of major depression.
Psychological risk factors for the development of postpartum depression
Risk factors can be grouped based on their importance to the occurrence of the condition. Depression and anxiety during pregnancy, postpartum blues, history of depression, neuroticism, excessive stress , marital disorders , lack of social support, and low self-esteem are strongly associated with postpartum depression. On the other hand, low socioeconomic status, not being married, unwanted pregnancy, labor difficulties, and infant restlessness have a relatively weaker association with the condition. The listed risk factors are more significantly related to the social and psychological aspects than to the biological aspects of the condition.
The exact mechanism for the development of postpartum depression is still not clear. There are many different models and theories explaining why the condition occurs over time. The biological model explains the development of postpartum depression as a result of the drastic and sudden decrease in the levels of many hormones , such as progesterone, estradiol and cortisol . In the withdrawal model, stress and reproductive hormones increase during pregnancy and drop dramatically during labor and the postpartum phase, leading to dysregulation of hormonal balance . The depressive model states the relationship of the condition to the dysregulation in the balance of stress hormones, mainly cortisol.
The role of dysregulation of the hypothalamic-pituitary axis in the genesis of the condition has also been suggested. Weakened dopaminergic regulation may also play a role. Many neuroendocrine changes during pregnancy may also influence the development of postpartum depression, including suppressed gamma-aminobutyric acid- GABA signaling and low levels of allopregnanolone. Psychological models focus mainly on the effect of pregnancy , childbirth and the onset of parenthood as the main stressors that cause symptoms of postpartum depression in women.
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7827176/